You are receiving this message as a subscriber to the FDA hepatitis electronic list serve. The purpose of the list serve is to relay important information about viral hepatitis-related products and issues, including product approvals, significant labeling changes, safety warnings, notices of upcoming public meetings and alerts to proposed regulatory guidances for comment.
Please do not reply to this message.
The U.S. Food and Drug Administration (FDA) is issuing updated recommendations concerning drug-drug interactions between drugs for human immunodeficiency virus (HIV) or hepatitis C virus (HCV) known as protease inhibitors and certain cholesterol-lowering drugs known as statins. Protease inhibitors and statins taken together may raise the blood levels of statins and increase the risk for muscle injury (myopathy). The most serious form of myopathy, called rhabdomyolysis, can damage the kidneys and lead to kidney failure, which can be fatal.
Facts about statins and protease inhibitors
- Statins are a class of prescription drugs used together with diet and exercise to reduce blood levels of low-density lipoprotein (LDL) cholesterol (“bad cholesterol”).
- HIV protease inhibitors are a class of prescription anti-viral drugs used to treat HIV.
- HCV protease inhibitors are a class of prescription anti-viral drugs used to treat hepatitis C infection.
- A side effect of taking HIV protease inhibitors is increased cholesterol and triglyceride (fat) levels. Therefore, some patients taking HIV protease inhibitors may need to take cholesterol-lowering medicines such as statins.
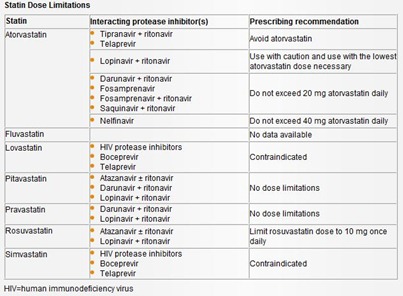
The labels for both the HIV protease inhibitors and the affected statins have been updated to contain consistent information about the drug-drug interactions. These labels also have been updated to include dosing recommendations for those statins that may safely be co-administered with HIV or HCV protease inhibitors (see Statin Dose Limitations below).
Healthcare professionals should refer to the current drug labels for protease inhibitors and statins for the latest recommendations on prescribing these drugs.
Patients should contact their healthcare professional if they have any questions or concerns about taking protease inhibitors and statins.
Additional Information for Patients
- Human immunodeficiency virus (HIV) and hepatitis C virus (HCV) protease inhibitors can interact with cholesterol-lowering statins to increase the risk of muscle injury.
- Patients should inform their healthcare professional about all medicines that they are taking or plan to take prior to starting an HIV or HCV protease inhibitor or statin.
- HIV and HCV protease inhibitors should never be taken (are contraindicated) with lovastatin (Mevacor) and simvastatin (Zocor) (see Statin Dose Limitations below).
- Patients should contact their healthcare professional if they have any questions or concerns about HIV or HCV protease inhibitors or statins.
- Patients should report side effects from the use of HIV or HCV protease inhibitors and/or statins to the FDA MedWatch program, using the information in the "Contact FDA" box at the bottom of the page.
Additional Information for Healthcare Professionals
- Co-administration of human immunodeficiency virus (HIV) or hepatitis C virus (HCV) protease inhibitors with certain statins can increase the risk of myopathy/rhabdomyolysis.
- Healthcare professionals should follow the recommendations in the drug labels when prescribing HIV or HCV protease inhibitors with statins (also see Statin Dose Limitations below).
- Healthcare professionals should report adverse events involving HIV or HCV protease inhibitors and/or statins to the FDA MedWatch program using the information in the "Contact FDA" box at the bottom of this page.
Atorvastatin
The results from a drug-drug interaction study with atorvastatin and lopinavir/ritonavir that were previously in the atorvastatin label have not yet been validated. Therefore, these results have been removed from the label and the dose cap of atorvastatin 20 mg when co-administered with lopinavir/ritonavir has also been removed. Pending validation of the study, healthcare professionals should use caution when co-administering atorvastatin with lopinavir/ritonavir and use the lowest necessary dose of atorvastatin.
Lovastatin and simvastatin
Lovastatin and simvastatin are sensitive in vivo cytochrome P450 3A4 (CYP3A4) substrates. Therefore, strong CYP3A4 inhibitors are predicted to significantly increase lovastatin and simvastatin exposures. A literature review indicates that itraconazole, a strong CYP3A4 inhibitor, increases lovastatin exposure up to 20-fold, and the drug interaction appears to result in rhabdomyolysis.1 Itraconazole increases simvastatin exposure up to 13-fold. Hence, other CYP3A4 inhibitors, including ketoconazole, posaconazole, erythromycin, clarithromycin, telithromycin, nefazodone, human immunodeficiency virus (HIV) protease inhibitors, and the hepatitis C virus (HCV) protease inhibitors boceprevir and telaprevir, are also expected to significantly increase lovastatin and simvastatin exposures. Therefore, concomitant administration of lovastatin and simvastatin with HIV protease inhibitors or HCV protease inhibitors (boceprevir and telaprevir) is contraindicated.
Rosuvastatin
The HIV protease inhibitor combinations lopinavir/ritonavir and atazanavir/ritonavir increase rosuvastatin exposure up to 3-fold. For these combinations, the dose of rosuvastatin should be limited to 10 mg.
- Lees RS, Lees AM. Rhabdomyolysis from the coadministration of lovastatin and the antifungal agent itraconazole. N Engl J Med. 1995;333:664-5.
Richard Klein
Office of Special Health Issues
Food and Drug Administration
Kimberly Struble
Division of Antiviral Drug Products
Food and Drug Administration
Source: Email from FDA
No comments:
Post a Comment